Donno V, Prats P, Rodriguez I, Polyzos NP.
Am J Obstet Gynecol. 2024 Oct 28:S0002-9378(24)01105-0.
DOI: 10.1016/j.ajog.2024.10.033
Accumulated evidence suggests that pregnancies following frozen embryo transfers in artificial cycles are associated with an increased risk of preeclampsia. Doppler ultrasonography of the uterine artery, along with maternal factors and serum biomarkers, is a crucial biomarker for first-trimester preeclampsia screening. It helps to identify “high-risk” patients. Guidelines strongly recommend administering aspirin (150 mg/day) to these women, due to solid evidence showing a 62% reduction in the incidence of preeclampsia.
Despite previous studies suggesting a lower uterine artery pulsatility index after frozen embryo transfers, no prior study has explored the impact of the type of endometrial preparation on uterine artery Doppler or its influence on estimating the risk of preeclampsia in the first trimester. For this reason, a group of researchers from the Reproductive Medicine Service at Dexeus Mujer decided to conduct a retrospective study to evaluate this.
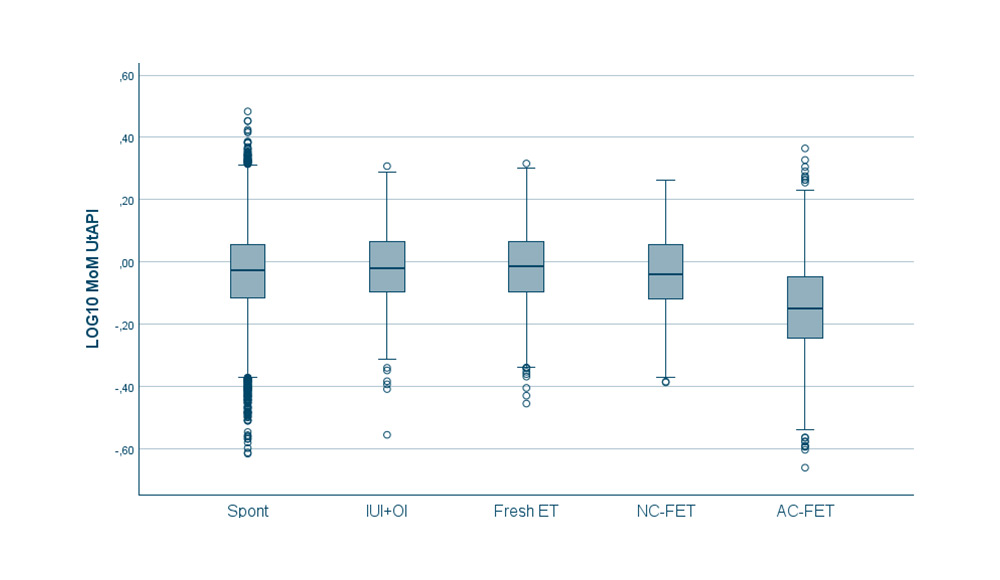
Led by Valeria Donno, the first author and a gynecologist specializing in assisted reproduction, the study included a total of 27,289 single pregnancies (conceived naturally or after assisted reproduction treatment) that underwent first-trimester ultrasound screening at the University Hospital from January 2010 to May 2023. The study aimed to assess whether there is an association between the uterine artery pulsatility index and the mode of conception, taking into account confounding factors (age, weight, smoking, and egg donation) in the multivariate analysis.
The results showed that pregnancies following artificial frozen embryo transfers presented a significantly lower uterine artery pulsatility index in the first trimester compared to other modes of conception. Moreover, the percentage of patients at high risk of preeclampsia in the first-trimester screening was significantly lower in the artificial cycle group compared to other groups. This resulted in a lower number of patients receiving prophylactic aspirin. The authors conclude that the first-trimester preeclampsia risk algorithm could be influenced by this variation in the uterine artery. In light of these findings, it is crucial to evaluate the possibility of adjusting this algorithm by incorporating correction factors to obtain a more accurate risk calculation and prevent untreated patients who could have benefited from prophylactic aspirin.
DEXEUS CAMPUS
Gran Vía de Carles III 71-75
08028 Barcelona
campus@dexeus.com
(+34) 93 227 47 09
® Copyright 2021-2025 Dexeus Mujer Foundation – Gran Via Carles III 71-75. 08028 Barcelona. Spain
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | This cookie is set by the GDPR cookie consent plugin. The cookie is used to store the user's consent for cookies in the "Analytics" category. | |
| cookielawinfo-checkbox-functional | The cookie is set by the GDPR cookie consent to record user consent for cookies in the "Functional" category. | |
| cookielawinfo-checkbox-necessary | This cookie is set by the GDPR cookie consent plugin. Cookies are used to store the user's consent for cookies in the "Necessary" category. | |
| cookielawinfo-checkbox-others | This cookie is used by the GDPR component. It is used to store the user consenting cookies in the "Other" category. | |
| cookielawinfo-checkbox-performance | This cookie is set by the GDPR cookie consent plugin. The cookie is used to store the user's consent for cookies in the "Performance" category. | |
| elementor | ||
| viewed_cookie_policy | The cookie is set by the GDPR cookie consent plugin and is used to store whether or not the user has consented to the use of cookies. It does not store any personal data. |
| Cookie | Duration | Description |
|---|---|---|
| _icl_visitor_lang_js | To allow multi-language functionality for web content. | |
| wpml_browser_redirect_test | Used to verify if cookies are allowed in the browser. |
| Cookie | Duration | Description |
|---|---|---|
| _ga | The _ga cookie, installed by Google Analytics, calculates visitor, session and campaign data and also tracks site usage for the site's analytics report. The cookie stores information anonymously and assigns a randomly generated number to recognize unique visitors. The _ga cookie, installed by Google Analytics, calculates visitor, session and campaign data and also tracks site usage for the site's analytics report. The cookie stores information anonymously and assigns a randomly generated number to recognize unique visitors. | |
| _ga_1WD9MFDMJK | This cookie is installed by Google Analytics. |
| Cookie | Duration | Description |
|---|---|---|
| wp-wpml_current_language | Necessary for the operation of the website in the different languages |